Lung Cancer Screening
On This Page
- What Is Screening?
- General Information About Lung Cancer
- Lung Cancer Screening
- Risks of Lung Cancer Screening
What Is Screening?
Screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
Scientists are trying to better understand which people are more likely to get certain types of cancer. They also study the things we do and the things around us to see if they cause cancer. This information helps doctors recommend who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarily think you have cancer if he or she suggests a screening test. Screening tests are given when you have no cancer symptoms.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
General Information About Lung Cancer
Key Points
- Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung.
- Lung cancer is the leading cause of cancer death in the United States.
- Different factors increase or decrease the risk of lung cancer.
Lung cancer is a disease in which malignant (cancer) cells form in the tissues of the lung.
The lungs are a pair of cone-shaped breathing organs in the chest. The lungs bring oxygen into the body as you breathe in. They release carbon dioxide, a waste product of the body's cells, as you breathe out. Each lung has sections called lobes. The left lung has two lobes. The right lung is slightly larger, and has three lobes. A thin membrane called the pleura surrounds the lungs. Two tubes called bronchi lead from the trachea (windpipe) to the right and left lungs. The bronchi are sometimes also involved in lung cancer. Tiny air sacs called alveoli and small tubes called bronchioles make up the inside of the lungs.

There are two main types of lung cancer: small cell lung cancer and non-small cell lung cancer.
Other PDQ summaries containing information related to lung cancer include:
Lung cancer is the leading cause of cancer death in the United States.
Lung cancer is the second most common type of non-skin cancer in the United States. Lung cancer is the leading cause of cancer death in men and in women.
Different factors increase or decrease the risk of lung cancer.
Anything that increases your chance of getting a disease is called a risk factor. Anything that decreases your chance of getting a disease is called a protective factor.
Tobacco smoking is the most important risk factor for lung cancer. Cigarette, cigar, and pipe smoking all increase the risk of lung cancer. Tobacco smoking causes about 9 out of 10 cases of lung cancer in men and about 8 out of 10 cases of lung cancer in women. The best way to prevent lung cancer is to not smoke.
For information about risk factors and protective factors for lung cancer, see Lung Cancer Prevention.
Lung Cancer Screening
Key Points
- Tests are used to screen for different types of cancer when a person does not have symptoms.
- Three screening tests have been studied to see if they decrease the risk of dying from lung cancer.
- Screening with LDCT scans has been shown to decrease the risk of dying from lung cancer in heavy smokers.
- Screening with chest x-rays and/or sputum cytology does not decrease the risk of dying from lung cancer.
- Screening tests for lung cancer are being studied in clinical trials.
Tests are used to screen for different types of cancer when a person does not have symptoms.
Scientists study screening tests to find those with the fewest harms and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) helps a person live longer or decreases a person's chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
Three screening tests have been studied to see if they decrease the risk of dying from lung cancer.
The following screening tests have been studied to see if they decrease the risk of dying from lung cancer:
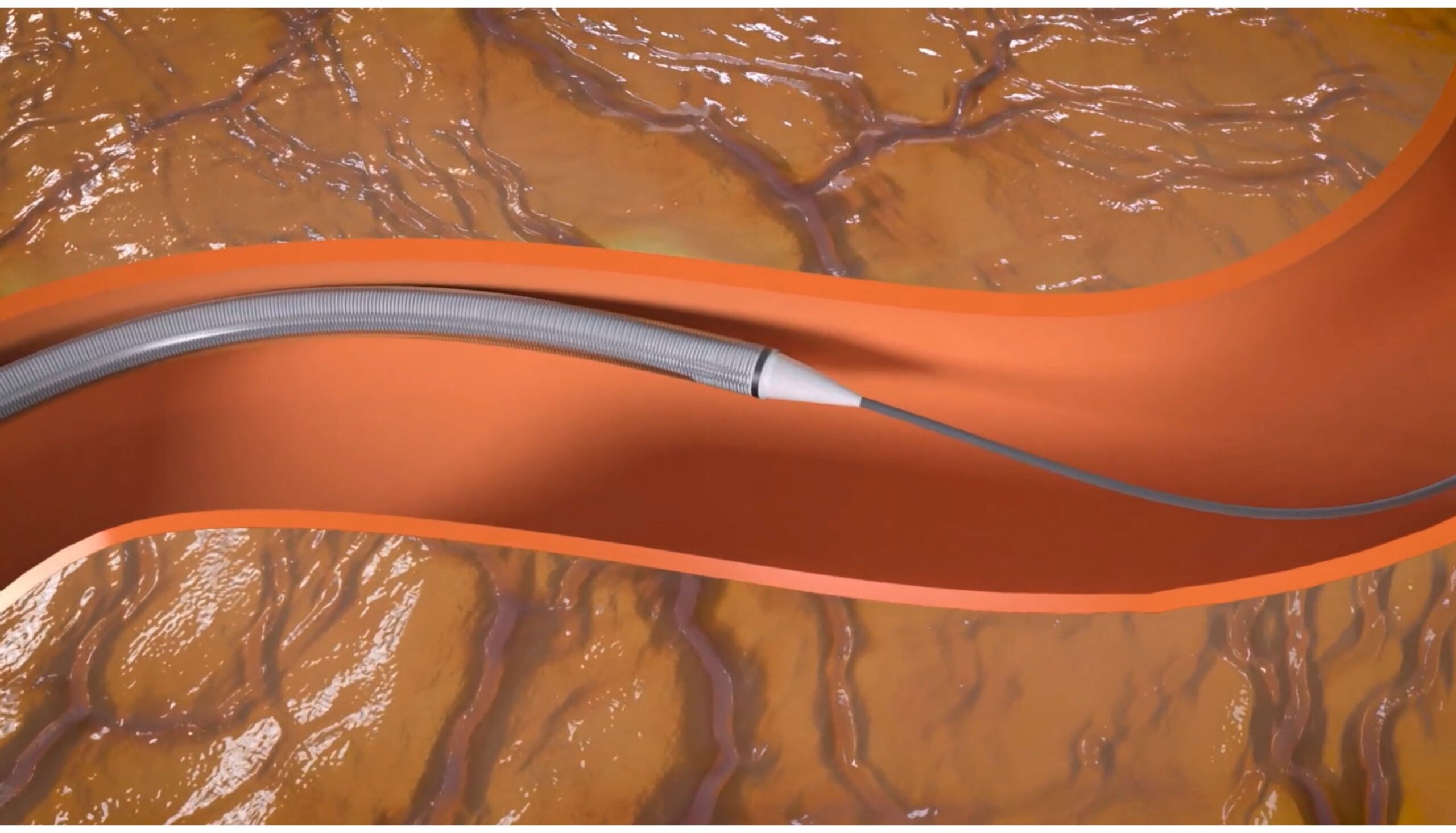
- Low-dose computed tomography (LDCT): A procedure that uses low-dose radiation to make a series of very detailed pictures of areas inside the body using an x-ray machine that scans the body in a spiral path. This procedure is also called spiral scan or helical scan.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Sputum cytology: Sputum cytology is a procedure in which a sample of sputum (mucus that is coughed up from the lungs) is viewed under a microscope to check for cancer cells.
Screening with LDCT scans has been shown to decrease the risk of dying from lung cancer in heavy smokers.
The National Lung Screening Trial studied people aged 55 years to 74 years who had smoked at least 1 pack of cigarettes per day for 30 years or more. Participants were either current smokers or former smokers who had quit within the last 15 years. The trial used chest x-rays or LDCT scans to check for signs of lung cancer.
Screening with LDCT once a year for three years was better than chest x-rays at finding early-stage lung cancer and decreased the risk of dying from lung cancer in current and former heavy smokers. Current smokers whose LDCT scan result shows possible signs of cancer may be more likely to quit smoking.
Screening with LDCT can cause possible harms, including:
- false-positive test results, which may lead to invasive procedures which are not needed
- overdiagnosis of some lung cancers, though it is not clear how often this happens
For more information about these possible harms, see the Risks of Lung Cancer Screening below.
A Guide is available for patients and doctors to learn more about the benefits and harms of screening for lung cancer.
Screening with chest x-rays and/or sputum cytology does not decrease the risk of dying from lung cancer.
Chest x-ray and sputum cytology are two screening tests that have been used to check for signs of lung cancer. Screening with chest x-ray, sputum cytology, or both of these tests does not decrease the risk of dying from lung cancer.
Screening tests for lung cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Risks of Lung Cancer Screening
Key Points
- Screening tests have risks.
- The risks of lung cancer screening tests include the following:
- Finding lung cancer may not improve health or help you live longer.
- False-negative test results can occur.
- False-positive test results can occur.
- Chest x-rays and CT scans expose the chest to radiation.
- Talk to your doctor about your risk for lung cancer and your need for screening tests.
Screening tests have risks.
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying from cancer.
The risks of lung cancer screening tests include the following:
Finding lung cancer may not improve health or help you live longer.
Screening may not improve your health or help you live longer if you have lung cancer that has already spread to other places in your body.
When a screening test result leads to the diagnosis and treatment of a disease that may never have caused symptoms or become life-threatening, it is called overdiagnosis. It is not known if treatment of these cancers would help you live longer than if no treatment were given, and treatments for cancer may have serious side effects. Harms of treatment may happen more often in people who have medical problems caused by heavy or long-term smoking.
False-negative test results can occur.
Screening test results may appear to be normal even though lung cancer is present. A person who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if there are symptoms.
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result (one that shows there is cancer when there really isn't) can cause anxiety and is usually followed by more tests (such as biopsy), which also have risks. A biopsy to diagnose lung cancer can cause part of the lung to collapse. Sometimes surgery is needed to reinflate the lung. Harms of diagnostic tests may happen more often in patients who have medical problems caused by heavy or long-term smoking.
Chest x-rays and CT scans expose the chest to radiation.
Radiation exposure from chest x-rays and low-dose CT scans may increase the risk of cancer. Younger people and people at low risk for lung cancer are more likely to develop lung cancer caused by radiation exposure from screening than to be spared death from lung cancer.
Talk to your doctor about your risk for lung cancer and your need for screening tests.
Talk to your doctor or other health care provider about your risk for lung cancer, whether a screening test is right for you, and about the benefits and harms of the screening test. You should take part in the decision about whether a screening test is right for you. For more information, see Cancer Screening Overview.